Surgical maculopathies: epiretinal membranes and full-thickness macular holes
Related content
Epiretinal membrane and full-thickness macular hole are common and treatable conditions of the retina. Left untreated, they can lead to profound loss of central vision, but with prompt and effective surgery, most patients will achieve significant improvements in visual acuity and distortion.
Surgery offers hope to patients affected by epiretinal membrane and full-thickness macular hole, both of which result in loss of central vision. Epiretinal membranes and full-thickness macular holes are both associated with vitreous detachment, usually in people during their 60s or 70s. It is important to recognise them as they can affect vision, and effective treatment is available. They often coexist with cataract, which may make them difficult to detect and lead to disappointing visual outcomes from cataract surgery.
How patients present
Patients with epiretinal membranes present with symptoms such as reduced central visual acuity, blurring, metamorphopsia (distortion of straight lines), aniseikonia (different-sized images) and loss of stereopsis. Vision loss is gradual and may not be noticed by patients.
Unlike epiretinal membranes, which come on quite slowly, patients with full-thickness macular holes present with fairly acute loss of central vision, as full-thickness macular holes occur quite rapidly. If a patient presents with reduced central vision and the lens is still relatively clear, it is mandatory to examine the macula and look for a full-thickness macular hole, as prompt diagnosis and referral can restore vision to normal. Full-thickness macular hole is three times more common in women than in men. Epiretinal membrane is also slightly more common in women. Large population-based studies found a prevalence of epiretinal membrane of between 7% and 11.8% using fundus photographs, but this increased to 34% when optical coherence tomography (OCT) was used. Full-thickness macular hole is less common, occurring in between 0.2 to 3.3 per 1,000 population.1 As both these conditions are uncommon in patients under 60, their prevalence will be lower in countries with a younger population.
Epiretinal membrane
Epiretinal membrane may be primary or secondary. Primary epiretinal membrane occurs when there is no risk factor other than a posterior vitreous detachment. Secondary epiretinal membrane occurs in conjunction with other eye diseases, most commonly diabetic retinopathy, retinal vein occlusion, or retinal tears/detachment.2
Clinical grading, based on photographs or slit lamp examination, may be divided into cellophane maculopathy, which is an early translucent epiretinal membrane without distortion of the retina, and macular pucker, or preretinal fibrosis, which is a more advanced form of epiretinal membrane, causing distortion of the inner retina.
How epiretinal membranes and macular holes develop
As people get older, the vitreous gel in the eye starts to degenerate. The posterior surface of the gel separates from the back of the eye and moves forward, towards the front of the eye. This is known as a posterior vitreous detachment. As the gel moves forwards, it can tear the peripheral retina, which can lead to retinal detachment.
Sometimes, a posterior vitreous detachment can result in conditions that affect central vision: epiretinal membrane and full-thickness macular hole.
In epiretinal membrane, the cells left behind or deposited on the surface of the retina after the vitreous detaches proliferate and – as the tissue contracts – this causes distortion and thickening of the macula.
The detaching vitreous may also pull on the fovea. A combination of anterior-posterior traction and tangential traction from the elastic internal limiting membrane results in a separation of all the layers of the retina, right through to the photoreceptor layer (outer retina), known as a full-thickness macular hole. There is no loss of retinal tissue, but the separation of retinal tissue means a loss of central vision. This can be restored if the hole is closed.
History and examination Enquire about diabetes, previous ocular trauma, and a history of flashing lights and floaters. Many patients with early epiretinal membrane are asymptomatic and the membrane may be identified at routine examination. Vision may be affected by traction, retinal oedema, or an opaque membrane.
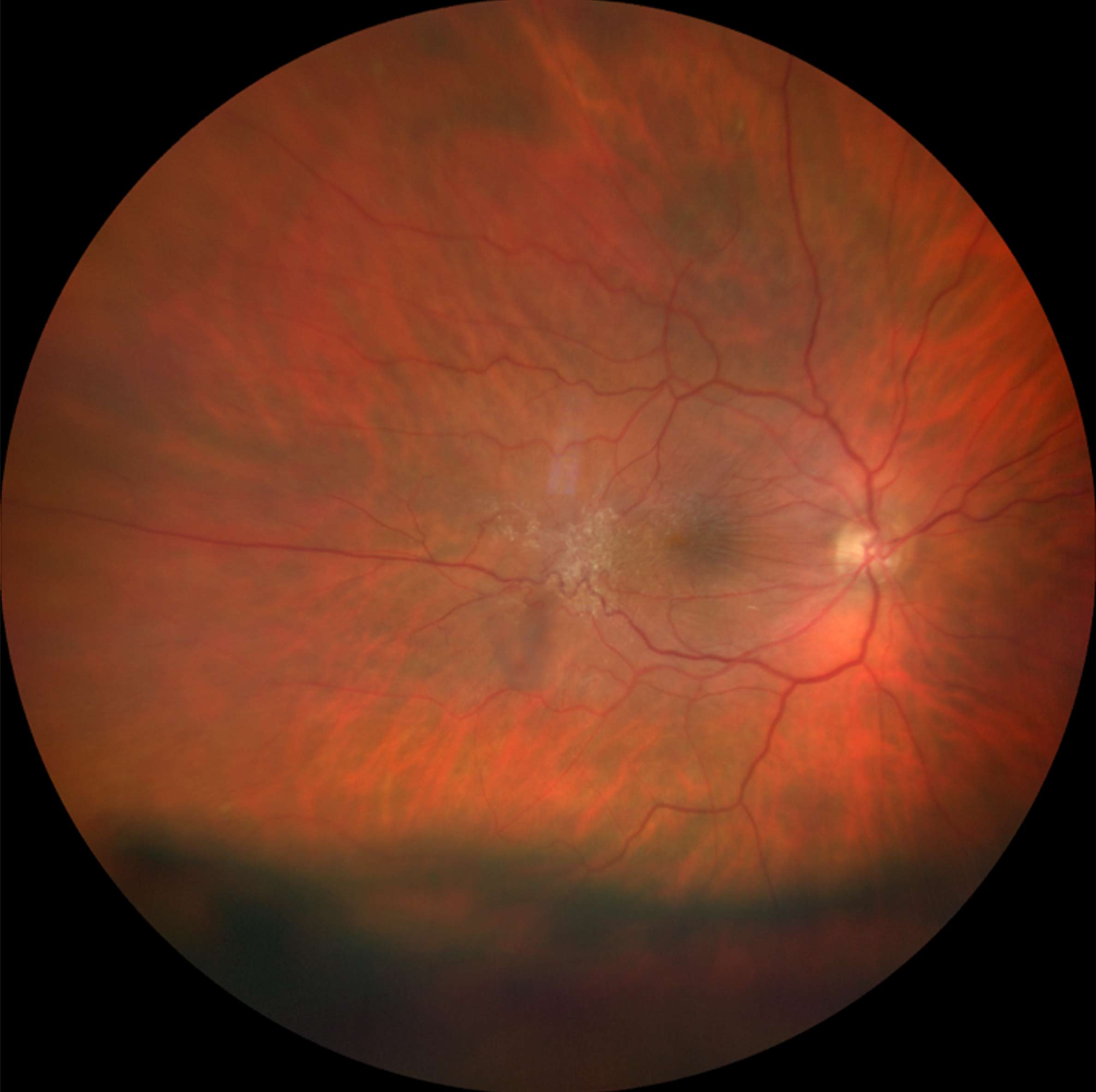
Early membranes can be seen as a glistening light reflex over the macula (Figure 1). As the membrane progresses, the retinal surface is wrinkled (Figure 2), and blood vessels become more tortuous or straightened. It may also be possible to detect cystoid macular oedema, loss of the foveal reflex, pseudoholes, and full-thickness macular holes. Investigations Optical coherence tomography (OCT) examination is invaluable in diagnosing, managing, and following patients with epiretinal membrane and macular holes. It is able to detect associated conditions like lamellar macular holes (a foveal cavity with undermined edges and loss of foveal tissue) and foveoschisis (separation of the foveal layers).

Treatment Most patients with epiretinal membrane will not require any treatment. Progression of epiretinal membrane is uncommon, and, if the patient is asymptomatic, they may be discharged and advised to return if their vision gets worse. Surgery for epiretinal membrane is performed when patients’ visual loss or symptoms affect their activities of daily living. The goal of surgery is to stabilise or improve vision and to reduce metamorphopsia. If you are unsure if a patient needs to be referred, ask them “Do you close your bad eye in order to see better with the good eye?” If they do, it is worth referring them to a retinal surgery centre.
Surgery consists of pars plana vitrectomy and removal of the epiretinal membrane, which may be combined with peeling of the internal limiting membrane. The surgeon uses a blue dye to stain the membranes and then peels them away from the macula with microforceps.
Complications All patients having vitrectomy for full-thickness macular hole or epiretinal membrane should be told that they will develop a cataract. Indeed, many surgeons combine cataract extraction with the vitrectomy. Patients should be warned of the risk of retinal detachment, haemorrhage, endophthalmitis, and hypotony, but these complications are rare.
Prognosis On average, vision improves by two lines of visual acuity. The greatest improvement is seen in patients with poor pre-operative visual acuity, but the final visual acuity is better in those with a better pre-operative visual acuity. Patients also get relief from metamorphopsia. The reduced distortion improves binocular vision, making it easier for the two eyes to work together. Patients usually report an improvement in their vision-related quality of life, even if there is only a small improvement in visual acuity. Following surgery, visual improvement is slow and may take up to 3 years.
Distinguishing pseudoholes from full-thickness holes
A pseudohole is a circular defect in the epiretinal membrane overlying the fovea, and it resembles full-thickness macular hole.
The visual acuity is usually 6/36 or worse in full-thickness macular hole, but rarely worse than 6/24 in pseudoholes. Always check the peripheral retina carefully to detect untreated retinal tears, and look for signs of vein occlusion or diabetic eye disease.
Full-thickness macular hole
Full-thickness macular hole is a defect in the fovea that involves all the neurosensory layers of the retina, from the internal limiting membrane down to the photoreceptor layer (Figure 3). Untreated, this is associated with severe central visual impairment. Full-thickness macular hole may be primary (caused during vitreoretinal detachment) or secondary. Causes of secondary full-thickness macular hole include trauma, severe myopia, and retinal detachment.
Diagnosis On presentation, depending on the duration of the macular hole, central visual acuity will range from 6/9 in very early, small holes, to counting fingers for long-standing, neglected holes. Macular holes can be diagnosed by careful slit lamp examination, but the signs are subtle (Figure 4). OCT scans are recommended.
Pathogenesis As the vitreous starts to detach, it pulls on the fovea. A combination of this antero-posterior traction and tangential traction from the elastic internal limiting membrane leads to a full thickness hole. The edges of the hole become hydrated, leading to macular oedema.3
Classification The International Vitreomacular Traction Study Group proposed OCT-based staging (Duker et al., 2013). The two stages depend on the presence (early stage) of vitreomacular traction or its absence (late stage). Further subgroups, based on size measured at the narrowest point of the hole, are: small (< 250 µm), medium (> 250 µm and < 400 µm), large (>400 µm). However, recent studies show that there is little difference in prognosis between 350 µm and 450 µm holes. We should therefore probably regard holes from 250-500 µm as medium, and large holes as any hole >500 µm.

Treatment Patients with recent-onset full-thickness macular hole, in particular, will benefit from prompt diagnosis and referral.
Surgery for full-thickness macular hole is similar to that for epiretinal membrane, with a few important differences. A posterior vitreous detachment often has to be induced. Triamcinolone acetonide microparticles can stain the vitreous, making it easier to see. Inducing a posterior vitreous detachment carries a risk of retinal tears. The peripheral retina must be inspected very carefully and any tears treated.
Peeling the internal limiting membrane has been proven to increase the success rate of full-thickness macular hole surgery. In large and refractory holes (holes that have not closed with surgery), internal limiting membrane flaps can be used to plug the hole to improve healing. Once the vitrectomy is completed, the eye is filled with a gas. Short-acting gases such as SF6 are used with smaller holes, while longer-acting gases such as C3F8 improve the outcome with larger holes. Maintaining a strict face-down position after surgery is difficult for most patients, and we have found that – as long as the eyes are looking down all the time, the outcome for small to medium holes is excellent without the patient needing to maintain a face-down posture. There is little benefit from maintaining an eyes-down or face-down posture for longer than 3 days, even for patients with larger holes.
Prognosis The prognosis is excellent for small/medium holes with a short duration. An estimated 95% of holes smaller than 500 µm are closed with a single operation. The average vision improvement is approximately 0.5 LogMAR units, equivalent to a change from 6/36 to 6/12. Large, chronic holes are more difficult to treat, and even when they are successfully closed, the vision may not improve as much.

References
1. Duker JS, Kaiser PK, Binder S, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120(12):2611-2619. doi:10.1016/j.ophtha.2013.07.042
2. Fung AT, Galvin J, Tran T. Epiretinal membrane: A review. Clin Exp Ophthalmol. 2021;49(3):289-308. doi:10.1111/ceo.13914
3. Premi E, Donati S, Azzi L, et al. Macular Holes: Main Clinical Presentations, Diagnosis, and Therapies. J Ophthalmol. 2022;2022:2270861. Published 2022 Apr 11. doi:10.1155/2022/2270861
