Pythium insidiosum: the organism that mimics fungal keratitis
Related content
Microbial keratitis is commonly caused by bacteria and fungi, however, what may appear to be fungal keratitis is sometimes the result of infection with a different microorganism: Pythium insidiosum.
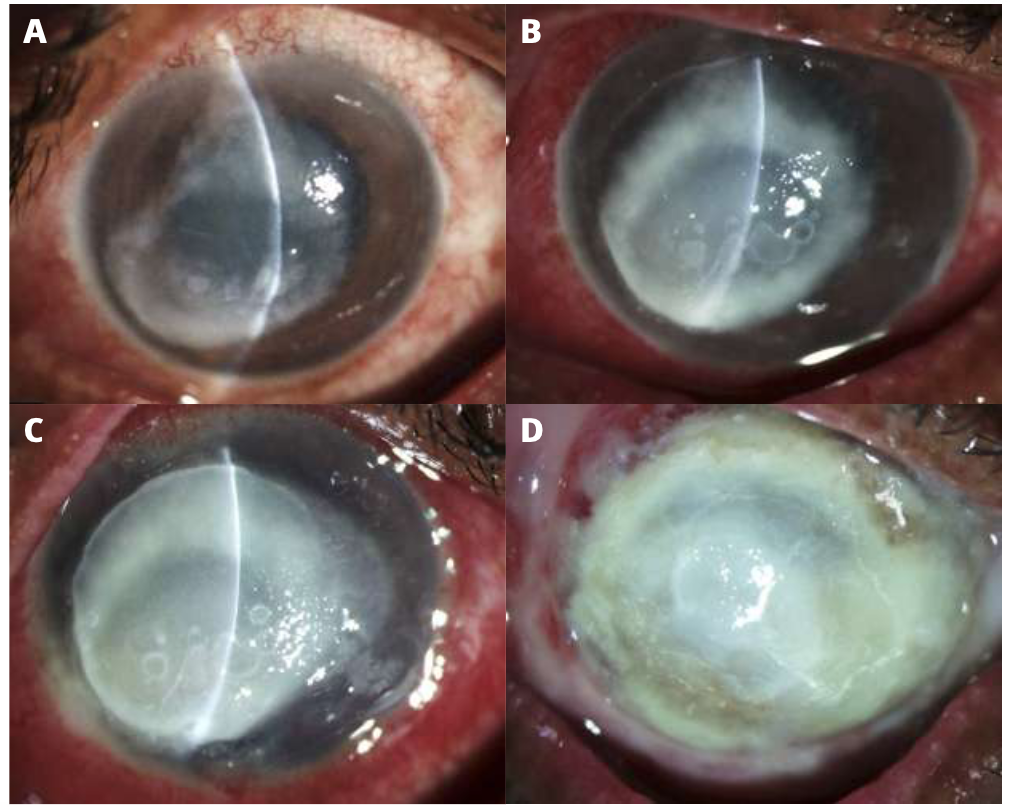
Pythium insidiosum belongs to a group of parasitic oomycetes, usually found in aquatic environments. Human infection is rare; however, a lack of awareness of Pythium spp. as a cause of microbial keratitis may lead to misdiagnosis as fungal keratitis and inappropriate treatment with antifungals. This has resulted in poor outcomes and the need to resort to therapeutic penetrating keratoplasty or evisceration (Figure 1).1,2
Pythium spp. produce spores and hyphal structures which led to them being misclassified as moulds until more recent genetic analysis proved otherwise.
The main reason it is important to differentiate Pythium infection from fungal infection is because the management is different – P. insidiosum is unresponsive to fungal treatment. Instead, it requires antibiotic treatment.
Microbial keratitis that looks like fungal keratitis (both clinically and on microscopy), but which does not respond to antifungal treatment, should be looked at again to rule out Pythium keratitis.
When to suspect Pythium keratitis
Although this type of corneal infection is more prevalent in subtropical and tropical climatic regions, the organism is widespread. Males are affected more frequently; this may be because they are more often exposed to ocular trauma during agricultural work. A significant proportion of patients affected have a history of dust or contaminated water in the eye(s), but there have also been reports of patients with a history of contact lens use and exposure to clay particles.
Signs, symptoms, and clinical findings
Affected patients usually complain of pain, redness, photophobia, and decreased vision on presentation.
The slit lamp findings3 include lid oedema and conjunctival congestion, a central or peripheral grayish-white infiltrate with a raised profile (Figure 1), hyphal-like projections, pinhead lesions in the anterior mid-stroma, and peripheral furrowing or guttering around the infiltrate. These features are suggestive of Pythium but may be present in some patients with fungal keratitis. Detailed microbiological workup is therefore necessary for diagnosis.


There may be associated scleritis and, rarely, endophthalmitis. Intraocular spread is rare, suggesting that the corneal barrier prevents posterior extension of the organism. Peripheral guttering or furrowing around the infiltrate is typically seen as the ulcer heals and the infiltrate size decreases (Figure 2).4,5 Significant, deep vascularisation is also seen in this phase.
Diagnosis
The diagnosis of Pythium keratitis requires a detailed microbiological workup by an experienced microbiologist.
Pythium filaments can be observed by direct microscopy of a corneal scraping in Gram stain, or in 10% potassium hydroxide (KOH) with 0.1% calcofluor white, viewed under fluorescence (Figure 3). The filaments are classically aseptate or sparsely aseptate,3 broad, and ribbon-like. However, this is also characteristic of some filamentous fungi or moulds, so further microbiological workup is needed to make a definitive diagnosis.

Pythium keratitis can be differentiated from fungal keratitis (including filamentous fungi or moulds) by staining a corneal scraping smear using a mixture of potassium iodide and iodine with 65% sulphuric acid (IKI-H2SO4). The slide must be examined immediately under the microscope. The P. insidiosum filaments are stained bluish-black, whereas fungal filaments appear yellowish.6 The growth on blood agar is feathery-edged and flat, and it is colourless or light brown (Figure 4). Further investigation includes growth of zoospores on carnation leaf pieces placed on non-nutrient agar and polymerase chain reaction (PCR).7
Treatment and management
Treatment is challenging as infection typically takes 2–3 months to resolve and patients may need to be admitted. Non-adherence could become an issue.
Patients presenting in the early or moderate stages of Pythium keratitis should be managed initially with a combination of antibiotics for a minimum of two weeks and observed closely. After the diagnosis is confirmed with a combined clinical and microbiological evaluation, start the patient on a combination of the following:
• Topical linezolid 0.2% (IV preparation) every hour during the day and every two hours at night
• Azithromycin 1% eye ointment twice a day
• Azithromycin 500 mg (orally) once a day for two weeks.
The combined topical medications are continued until a response is noted in the form of scarring or decrease in the size of infiltrate. With timely medical intervention, more than 70% cases can be successfully managed.3
Most patients can be seen as outpatients with regular follow-up. Patients who may have difficulty adhering with treatment, those who live far away, and those with only one functioning eye are admitted for 1–2 weeks.
Examine patients clinically every three days, followed by once a week, to assess the response. Check for thinning and deeper extension of infiltrate, including limbal infection, as this suggests the infection might be moving beyond the cornea, and could then spread more widely.
Good response to medical treatment is evident from the decrease in the size of hyphal-like extensions (Figure 5) and cellularity of the surrounding stroma.
Poor response to medical treatment includes:
• Thinning. Plan cyanoacrylate glue application in patients with significant corneal thinning to avoid corneal perforation.
• Extension of the infiltrate and limbal infection. Consider therapeutic penetrating keratoplasty.
Patients presenting with advanced Pythium keratitis need close supervision and should be admitted and seen daily. Therapeutic penetrating keratoplasty with an extra 1.5 mm margin may be needed, as medical treatment alone may not be sufficient for the eradication of infection. Unfortunately, this modality is associated with a high risk of recurrence of infection, and evisceration may eventually be necessary.
The combined topical medications are continued until a response is noted in the form of scarring or decrease in the size of infiltrate. With timely medical intervention, more than 70% of patients can be successfully managed.3

Follow-up care On the resolution of keratitis, there are increased chances of the development of cataract and glaucoma, which can significantly delay visual recovery, in addition to causing corneal scarring to develop. The development of cataract can be secondary to severe inflammatory reactions due to long-standing infection. Many of these patients need optical keratoplasty and cataract surgery for visual rehabilitation. The outcomes of these grafts are similar to grafts done for other indications.
References
1. Agarwal S, Iyer G, Srinivasan B, Benurwar S, Agarwal M, Narayanan N, et al. Clinical profile, risk factors and outcome of medical, surgical and adjunct interventions in patients with Pythium insidiosum keratitis. Br J Ophthalmol. 2019;103(3):296-300.
2. Hasika R, Lalitha P, Radhakrishnan N, Rameshkumar G, Prajna NV, Srinivasan M. Pythium keratitis in South India: Incidence, clinical profile, management, and treatment recommendation. Indian J Ophthalmol. 2019 Jan;67(1):42-7.
3. Sharma S, Balne PK, Motukupally SR, Das S, Garg P, Sahu SK, et al. Pythium insidiosum keratitis: clinical profile and role of DNA sequencing and zoospore formation in diagnosis. Cornea. 2015;34(4):438-42.
4. Bagga B, Sharma S, Madhuri Guda SJ, Nagpal R, Joseph J, Manjulatha K, et al. Leap forward in the treatment of Pythium insidiosum keratitis. Br J Ophthalmol. 2018;102(12):1629-33.
5. Bagga B, Kate A, Mohamed A, Sharma S, Das S, Mitra S. Successful strategic management of Pythium insidiosum keratitis with antibiotics. Ophthalmology. 2021;128(1):169-72.
6. Mittal R, Jena SK, Desai A, Agarwal S. Pythium Insidiosum Keratitis: Histopathology and Rapid Novel Diagnostic Staining Technique. Cornea. 2017 Sep;36(9):1124-1132.
7. Behera HS, Barik MR, Das S, Sharma S. Simple polymerase chain reaction assay to differentiate between fungal and Pythium insidiosum keratitis. Clin Exp Ophthalmol. 2021;49(6):630-632.
