Management of myopic traction maculopathy
Related content
High myopic eyes with myopic traction maculopathy were expected to improve only anatomically after surgery. With early detection and appropriate treatment, however, visual acuity can improve by an average of two lines.
Myopia, or short sightedness (defined as more than or equal to 0.50 D of myopia) is the leading cause of refractive error, affecting 35% of the population in 2023.sup>1
Genes have been identified for myopiasup>2-5 that are thought to determine one’s susceptibility to environmental factors, including too much time spent on near work,sup>5 insufficient time spent outdoors, low levels of vitamin D,sup>6 inadequate light exposure, and poor diet. There is evidence emerging that increased time spent outdoors can reduce the risk of developing myopia and – in those with myopia – it can reduce the rate of progression.sup>5
High myopia, defined as refractive error above 6 diopters (D) and/or axial length above 26.5 mm (an eyeball longer than normal), affects a growing number of people worldwide, with the highest rates in urban Asian countries (5–9%).sup>6



The progressive elongation of the myopic eye leads to three main consequences at the back of the eye: atrophy, neovascularisation, and tractional changes; collectively, these are known as myopic maculopathy.
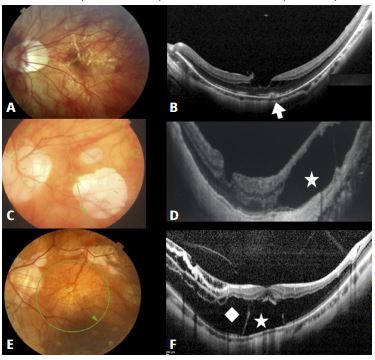
1. Atrophy indicates thinning of the choroid. The choroid, stretched by the elongation of the eye, breaks, creating lacquer cracks (see Figure 1 a and b), and then disappears (atrophy, see Figure 1, c and d). This complication is untreatable
2. Neovascularisation is the formation of new vessels from the choroid to the retina (Figure 1b and Figure 2). This complication is treatable with intravitreal anti-VEGF injections.
3. Tractional changes in the retina, (Figure 1e and f, and Figure 3) are known as myopic traction maculopathy (MTM); this may affect up to 30% of eyes with high myopia.
Myopic traction maculopathy
Myopic traction maculopathy (MTM) is the term used to describe the different tractional effects on the macula due to the elongation of the eye as a result of high myopia. MTM may affect up to 30% of eyes with high myopia,sup>2,3 especially if a posterior staphyloma is present as an ectasia (or bulging) in the posterior eyewall. The ectasia of the posterior eyewall is visible with widefield OCT or magnetic resonance imaging (MRI), as shown in Figure 4.
MTM is considered a complex disease. But everything is complex only when it is not fully understood.
Until 2020, there was no comprehensive classification in the literature,sup>4,5,7 very limited information on pathogenesis and natural history, and no consensus on the complete terminology of the different types of myopic traction maculopathy, nor on treatment.
We analysed hundreds of OCT images of highly myopic eyes, affected by different stages of MTM, over a very long period and then published the MTM staging system (Figure 5). This divides MTM not in types but in stagessup>8, to highlight the dynamic and continuously evolving nature of the disease. Next, we offered guidelines on the type and timing of management, customised for each stage.
The stages of MTM As the eye elongates and enlarges in progressive myopia, the macula might show signs of anteroposterior traction (traction perpendicular to the foveal plane) and tangential traction (traction at an angle to the foveal plane).
The four rows in the MTM staging system (Figure 5) represent the evolution of the disease in a direction perpendicular to the retina: from inner/outer schisis (splitting of the retinal layers) (stage 1) to predominantly outer schisis (stage 2) to schisis-detachment (stage 3) to complete macular detachment (stage 4). The three columns represent the evolution in a direction tangential to the retina and the fovea: from normal fovea (stage a) to inner lamellar macular hole (stage b) to full-thickness macular hole (stage c).
The outer lamellar macular hole is marked as O and might occur in stage 2, 3, or 4.
The presence of epiretinal abnormalities is marked as + (read as “plus”) and might occur in every stage.
The retina can evolve from stage 1 to stage 4 and from pattern a to c simultaneously or separately. The mean time taken to evolve from one stage to the next is marked in Figure 5, as well as the average visual acuity.
MTM stages might show a spontaneous improvement.sup>4 However, we determined that, when the eyes are followed for a long time, MTM might start to evolve once again, even after spontaneous resolution.

How we diagnose myopic traction maculopathy Indirect ophthalmoscopy and biomicroscopy can identify pathologic myopia but not MTM. OCT is the key instrument to diagnose this disease.sup>1,9 In fact, the true description of MTM began with the advent of OCT.sup>1
When OCT is not available, and the vision is good, we cannot exclude that MTM could be already present. However, usually in early stages, like stages 1a, 1b, 2a, 2b (Figure 5) vision is still in the range of 0,5–1,0 decimal, in the absence of macular atrophy.
When vision starts to decrease in the absence of atrophy, neovascularisation, and haemorrhages, we should suspect MTM in the form of stage 3, 4, or any stage c, even in the presence of a normal fundus appearance, as shown in Figure 1 e and f. These patients should be referred for OCT.
Ideally, all patients with high myopia should be referred for an OCT, if available, no matter what level of vision they have, in order to identify possible myopic maculopathy, classify the stage of myopic maculopathy (if present) and offer appropriate advice for future management.
How we manage myopic traction maculopathy
Our studies show that, to obtain the best efficacy to safety ratio, patients in the early stages of myopic traction maculopathy, with intact fovea and good vision, should be observed, since progression is slow. For patients with more advanced disease, treatment is required:
• MTM, in the form of schisis and detachment of the macula, can be counteracted by placing a macular buckle which pushes the sclera towards the retina, solving the schisis and detachment.
• Lamellar or full thickness macular hole can be counteracted by pars plana vitrectomy (PPV) which creates a force pointing toward the centre of the fovea.
In summary, when vision is good, the patient should just be observed but with periodic OCT. In the presence of a macular detachment, a macular buckle should be applied.
If a macular hole is present, consider vitrectomy.
One great advantage of using a macular buckle to solve the schisis and detachment secondary to MTM is that it avoids the use of silicone oil, often proposed when treating recurrent retinal detachments in MTM. Standard or heavy silicone oil in highly myopic eyes inevitably leads to secondary glaucoma.
Macular buckle The macular buckle is a device that shortens the eye. The surgical technique aims to counteract the pulling effect exerted on the retina by the elongation of the sclera. The buckling side of the device is placed behind the posterior pole, in order to push the sclera anteriorly.
Different models of macular buckle have been proposed.10 Surgery may be performed under general or local anaesthesia. For local anaesthesia, we prefer sub-Tenon’s anaesthesia with a blunt cannula to avoid the potential risk of scleral perforation with a retrobulbar injection in highly myopic eyes. The surgical technique is shown in this video: https://youtu.be/WdIjLCHbYtE
When following these guidelines, the prognosis of surgery is good, and the best corrected visual acuity improves with an average of 2 lines. It is particularly important to highlight this achievement, because, currently, high myopic eyes with myopic traction maculopathy are expected to improve only anatomically, not functionally, after surgery.sup>11
References
1. Pu Y, Chen J, et al. Global prevalence, trend and projection of myopia in children and adolescents from 1990 to 2050: a comprehensive systematic review and meta-analysis. Br J Ophthalmol. Published online September 24, 2024. doi:10.1136/bjo-2024-325427
2. Baba T, Ohno-Matsui K, Futagami S, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003;135(3):338-342. doi:10.1016/s0002-9394(02)01937-2
3. Benhamou N, Massin P, Haouchine B, Erginay A, Gaudric A. Macular retinoschisis in highly myopic eyes. Am J Ophthalmol. 2002;133(6):794-800. doi:10.1016/s0002-9394(02)01394-6
4. Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013;156(5):948-957.e1. doi:10.1016/j.ajo.2013.06.031
5. Shimada N, Ohno-Matsui K, Yoshida T, Sugamoto Y, Tokoro T, Mochizuki M. Progression from macular retinoschisis to retinal detachment in highly myopic eyes is associated with outer lamellar hole formation. Br J Ophthalmol. 2008;92(6):762-764. doi:10.1136/bjo.2007.131359
6. Matsumura S, Ching-Yu C, Saw SM (2020). Global Epidemiology of Myopia. In: Ang M, Wong T (eds) Updates on Myopia. Springer, Singapore. https://doi.org/10.1007/978-981-13-8491-2_2
7. Ruiz-Medrano J, Montero JA, Flores-Moreno I, Arias L, García-Layana A, Ruiz-Moreno JM. Myopic maculopathy: Current status and proposal for a new classification and grading system (ATN). Prog Retin Eye Res. 2019;69:80-115. doi:10.1016/j.preteyeres.2018.10.005
8. Parolini B, Palmieri M, Finzi A, et al. The new Myopic Traction Maculopathy Staging System. Eur J Ophthalmol. 2021;31(3):1299-1312. doi:10.1177/1120672120930590
9. Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol. 2007;125(6):767-772. doi:10.1001/archopht.125.6.767
10. Parolini B, Frisina R, Pinackatt S, Mete M. A new L-shaped design of macular buckle to support a posterior staphyloma in high myopia. Retina. 2013;33(7):1466-1470. doi:10.1097/IAE.0b013e31828e69ea
11. Parolini B, Palmieri M, Finzi A, Frisina R. Proposal for the management of myopic traction maculopathy based on the new MTM staging system. Eur J Ophthalmol. 2021;31(6):3265-3276. doi:10.1177/1120672120980943
12. Takai Y, Tanito M, Sugihara K, Kodama T, Ohira A. Temporal inverted internal limiting membrane flap technique for a macular hole patient unable to maintain postoperative prone positioning. Retin Cases Brief Rep. 2016;10(4):323-326. doi:10.1097/ICB.0000000000000258
